


The Radiology Department employs an array of advanced medical devices to diagnose a variety of diseases. These devices are instrumental in facilitating precise imaging and accurate assessments, allowing for effective treatment planning. The equipment used includes:
A. DEVICES THAT USES X-RAY (MAY BE HAZARDOUS IN PREGNANCY)
1. X-Ray
2. Mammography
3. Bone Densitometry
4. Computerized Tomography (CT),
5. Angiography = DSA = Digital subtraction angiography = Catheter angiography

Ultrasound
a. This medical device is primarily used for diagnosing diseases in intra-abdominal organs.
b. It also plays a crucial role in monitoring pregnancies and is recognized for its safety.
Color Doppler Ultrasound
a. Employed for diagnosing vascular diseases.
b. Evaluates the blood supply to various organs.
c. Frequently used during pregnancy to monitor fetal development.


Conventional Computerized Tomography (CT)
Conventional CT utilizes a scanner equipped with an X-ray tube and detectors. The patient lies between these components, allowing X-rays to pass through the body and be captured by the detectors. As different tissues absorb X-rays variably due to their atomic densities, detailed cross-sectional images are created. During the scanning process, the tube and detectors rotate 360 degrees around the patient. After each image is captured, the table moves forward to acquire the next slice. This method, while comprehensive, is time-consuming and sensitive to respiratory movements, limiting its suitability for cardiovascular studies.
Spiral Computerized Tomography (Spiral CT)
Spiral CT has been developed to address the limitations of conventional CT. In this approach, the X-ray tube and detectors continuously rotate around the patient, who is simultaneously moved along the table at a predetermined velocity, following a spiral path. This advancement significantly reduces the time required for examinations, although it remains less effective for imaging moving organs such as the heart.

Multi-Slice Computerized Tomography (MS CT)
To further enhance imaging capabilities, multi-slice spiral CTs have been introduced. These scanners feature thinner detectors arranged in multiple rows, with advancements allowing for up to 64 rows in the latest models. This configuration improves image resolution and enables faster data acquisition, allowing patients to hold their breath for shorter periods, typically less than 20 seconds.
Advantages of Multi-Slice Computerized Tomography
Disadvantages of Multi-Slice Computerized Tomography

Color Doppler Ultrasound
Color Doppler Ultrasound is based on the Doppler effect, where the frequency of sound waves changes as they echo from moving structures, such as red blood cells. This method is instrumental in evaluating blood flow within vascular structures. Flow data is color-coded relative to the transducer's direction and velocity, and integrated into grayscale images of blood vessels to produce color Doppler images. Velocity and flow patterns are analyzed using graphical Doppler spectra.
Applications of Doppler Ultrasound
Doppler Ultrasound is versatile, used for assessing arterial and venous structures in various body regions, detecting vascular occlusions, and evaluating vascularization in tumors and inflammatory formations. It is also pivotal in prenatal screenings and assessing the vascular health of gynecological tumors and transplanted organs. The Logic 7 device, equipped with advanced sonography technology, ensures high-quality imaging through features like coded harmonic imaging and automated tissue optimization.
Role of Ultrasound in Trisomy Screening
Ultrasound plays a critical role in the first-trimester screening for chromosomal anomalies. It measures the nuchal translucency of the fetus, along with other fetal structures, to assess the risk of trisomy. Doppler ultrasound additionally evaluates the fetal heart and umbilical cord. Following the ultrasound, blood tests analyze specific markers, and the combined results are used to estimate the likelihood of chromosomal abnormalities.

Types of Doppler Ultrasound
Doppler ultrasound employs two primary modes to analyze blood flow within vessels. The first mode, known as Color Doppler, integrates color coding into conventional ultrasound images to depict blood flow; vessels are marked in red to indicate flow towards the probe and blue to denote flow away from it. The second mode, Spectral Doppler, presents blood flow data in a graphical format—distinct from standard ultrasound imagery. This mode produces flow curves, each displaying unique characteristics dependent on the specific vessel being examined. Once an image is captured and the target vessel identified, Spectral Doppler is activated to focus on that vessel, enabling precise mathematical calculations of blood flow velocity and vascular resistance.
Due to their high cost, ultrasound scanners equipped with Doppler capabilities are not universally available, often necessitating separate Doppler examinations conducted by specialists other than those overseeing the primary ultrasound, such as in prenatal care. Furthermore, it is important to differentiate between detailed ultrasound scans—commonly but inaccurately referred to in colloquial terms as “color ultrasounds”—and Doppler scans, as the former requires specialized training and experience.

Utility of Doppler Scans
Doppler scans are invaluable for assessing blood supply to tissues, crucial for the maintenance of tissue viability through oxygen and nutrient delivery and waste removal. For instance, in conditions like ovarian torsion, where the ovary twists around its axis potentially leading to gangrene from insufficient blood supply, Doppler scans can critically determine the adequacy of blood flow, thus influencing surgical decisions. Similarly, in oncology, Doppler scans help identify hypervascularization in tumors, aiding in the differentiation between benign and malignant pathologies through the visualization of neovascularization.
In prenatal care, Doppler scans are instrumental in monitoring placental and fetal health. They assess the vascular resistance in uterine and umbilical arteries, providing insights into potential complications such as pre-eclampsia, intrauterine growth retardation, and early placental separation. Notably, Doppler screening at 20 weeks of pregnancy is recommended for high-risk cases, as it can predict complications by analyzing changes in blood flow and resistance. These findings, especially noted deviations in Doppler flow curves, can necessitate immediate and intensive monitoring.
Moreover, Doppler ultrasound is pivotal in the early detection of fetal heartbeats and in visualizing major fetal arteries, contributing to the comprehensive evaluation of fetal well-being and the identification of potential anatomical anomalies. As such, the strategic application of Doppler ultrasound is critical in both emergency and routine prenatal settings, ensuring timely medical interventions and ongoing fetal health assessment.

Doppler ultrasound scanning does not necessitate a separate session. Should the ultrasound equipment employed during routine pregnancy check-ups be equipped with Doppler capabilities, your physician can activate this feature at any time to observe and assess blood flow. For instance, during a typical first ultrasound at six weeks of pregnancy, where fetal heartbeats are monitored, Color Doppler can subsequently be utilized to visualize vascular structures adjacent to the fetal urinary bladder. Around the 20th week of pregnancy, during a detailed ultrasound, the physician may evaluate the blood flow in the arteries supplying the uterus if necessary. In later routine scans, the focus shifts to assessing blood flow in the umbilical cord and monitoring the overall health of the fetus.
Are There Risks Associated with Doppler Scans?
From a theoretical standpoint, Doppler ultrasound may pose a slightly higher risk than regular ultrasounds due to potential regional increases in heat and the risk of aneurysm. However, despite animal studies indicating that prolonged Doppler usage could result in tissue temperature increases of approximately 2.5°C, such levels remain safe for humans, and obstetric Doppler scans are not typically of long duration. To date, there have been no reported adverse effects from Doppler scans on humans.

Bone Densitometer and Technical Data
A bone densitometer measures bone density, aiding in the assessment of bone fragility. If osteoporosis is diagnosed, this tool is also instrumental in monitoring the efficacy of medicinal treatments. The measurement process takes only one minute. Often referred to as "the silent disease," osteoporosis may not cause pain, leading patients to inadvertently neglect their medication, thereby worsening their condition silently. Although considered untreatable, osteoporosis progression can be halted with appropriate medication and lifestyle adjustments.
Should I Have My Bone Density Measured?
Bone densitometry is advisable for individuals between the ages of 20-45 to have a baseline measurement, as bone loss can commence without noticeable symptoms until significant pain or fractures occur at more advanced ages. Vertebral depressions often go unnoticed in everyday activities.

How Frequently Should Bone Densitometry be Measured?
The frequency of bone densitometry tests depends on the extent of bone density loss, the treatment regimen, and any ongoing conditions that may affect bone health. Your physician will guide the necessary follow-up schedule based on these factors.
What is Osteoporosis?
Osteoporosis is a skeletal condition that predominantly affects women post-menopause and men over the age of 55, characterized by reduced bone mass and the deterioration of bone tissue structure, which increases the risk of fractures. This condition results from the natural decrease in calcium levels and is irreversible, though its progression can be managed if diagnosed early. While commonly associated with menopausal women due to decreased estrogen levels, osteoporosis can also affect younger individuals and men for various reasons.

How is Bone Structure Formed?
Bone is a dynamic tissue consisting of a compact outer layer and a spongy inner layer, influenced by genetic factors, acquired diseases, and lifestyle choices such as diet, physical activity, and exposure to sunlight. Factors like multiple pregnancies, prolonged immobilization in work settings, certain medical conditions, and long-term medication use can also impact bone development.
Changes in Bone Structure Due to Osteoporosis: In the initial stages of osteoporosis, the compact (hard) layer of bone becomes thinner, and the spaces within the spongy layer enlarge. As the condition progresses, weakened bones are prone to fractures, particularly in advanced ages.
Consequences of Osteoporosis: Osteoporosis can significantly alter the structure of vertebral bones, leading to a shortened stature and a humpback appearance. Fractures in the hip, wrist, ankle, and spine are common and can occur from minimal trauma.
Symptoms of Osteoporosis: Typically, osteoporosis does not present with noticeable symptoms or pain until a fracture occurs. However, some individuals may experience bone pains, often misdiagnosed as rheumatism in later years. Advanced stages of bone loss can result in significant pain, collapsed vertebrae, decreased height, and increased instances of fractures in the hip, hand, and wrist. Notably, bone loss can be detected incidentally during an X-ray, which might reveal up to a 45% loss before diagnosis, underscoring the critical role of bone densitometry as the sole diagnostic and monitoring tool for osteoporosis.
Osteoporosis is not exclusively a condition affecting women and the elderly but is widespread across various demographics. Advanced age fractures impose substantial financial burdens on patients, their families, and social security systems. Affected individuals often experience a decline in quality of life, and those with femoral fractures may face significantly reduced life expectancy. Ideally, everyone should undergo an initial screening and subsequent annual follow-ups if osteoporosis is confirmed, or biennially if osteopenia is detected, with further assessments tailored by physicians based on age and gender. Patients undergoing renal dialysis should receive biannual evaluations due to accelerated bone loss associated with chemical treatments.

Bone Mineral Densitometry Measurement Techniques: Bone mineral density measurements are critical for diagnosing osteoporosis, assessing fracture risk, determining the need for treatment, and monitoring therapy effectiveness. An ideal densitometric measurement is quick, reliable, minimally invasive, and capable of distinguishing between trabecular and cortical bone structures.
Dual Energy X-ray Absorptiometry (DEXA): A more recent and rapid technique that utilizes X-rays to measure the lumbar region, femur, or entire body. DEXA provides precise measurements with a minimal radiation dose and is capable of producing detailed images quickly.

Osteoporosis risk groups include:

Osteoporosis can now be diagnosed even with minimal bone loss, such as 1%, using bone densitometry measurements. Diagnosis primarily begins with a thorough medical history and physical examination. This history may include questions about any past osteoporosis-related medical conditions, personal or familial history of fractures, and more. Physicians may recommend X-rays to detect any fractures and a bone densitometry test to determine bone mineral density after conducting physical exams and other tests.
Bone densitometry is a painless process similar to undergoing an X-ray. During this procedure, the mineral density of the targeted bone areas is measured using X-ray beams and sound waves. The results are then compared with the bone mineral density values of healthy young adults to calculate a T-score, which helps determine the condition of the bones compared to those of healthy individuals.

The most advanced method used in bone density measurements is Dual X-ray Absorptiometry (DPX-DEXA). The LUNAR-DPX-DEXA system, noted for its high accuracy, is compliant with Turkish standards and is endorsed by the World Health Organization (WHO). The resulting T-score is reported, and the risk of fracture is graphically depicted as per WHO guidelines. Additionally, percentage changes in recurrent measurements are monitored, and responses to therapy are tracked.
Proposed Changes for the Lunar-DPX-NT Bone Density Measurement Device:
The Lunar-DPX-NT device is designed for precise bone density measurements, including AP Spine Femur, Whole Body, Dual Femur, Forearm, and Lateral Spine. Additionally, it can swiftly provide body composition assessments (including fat ratio) with excellent repeatability.
Indications for Bone Densitometry Testing:
Bone densitometry should be performed considering the patient's risk factors and only if the results will aid in therapeutic decisions. For individuals undergoing hormone replacement therapy for menopause, further bone densitometry may be redundant. However, conducting a bone density test prior to therapy can offer valuable insights into personal risk levels and assist in therapeutic decisions. Regular bone densitometry tests every 18-24 months can be useful for monitoring therapy response.

Osteoporosis prevention can be achieved through lifelong habits established from childhood. Key preventive measures include maintaining adequate calcium intake, regular physical activity, and hormone levels (estrogen in women, testosterone in men). Achieving strong bone density during childhood and adulthood provides substantial protection against future osteoporosis. Lifestyle choices such as avoiding smoking, maintaining a healthy body weight, and limiting alcohol are crucial. Bone mass reaches its peak in the 20s and gradually declines over the next 20 years. Factors like low dietary calcium, vitamin D deficiency, smoking, excessive alcohol consumption, a sedentary lifestyle, or medications that affect bone metabolism can accelerate bone loss, especially in older adults.
Bone Density Measurement Indications for Pediatricians (Ages 5-20):


For Physiotherapists:

For Orthopaedists:


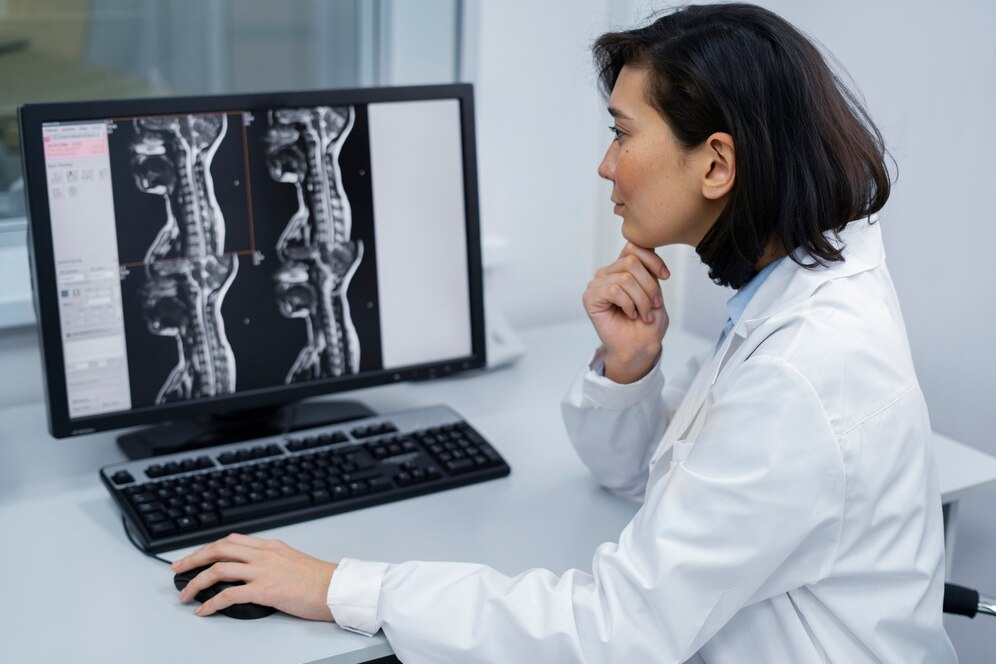
Magnetic Resonance Imaging (MRI) is a non-invasive diagnostic technique that provides high-resolution images of internal body structures without the use of harmful X-rays. This method utilizes radio waves and a strong magnetic field to excite hydrogen atoms in the body, producing detailed images, particularly of soft tissues. MRI does not require the use of iodinated contrast agents, which can cause allergic reactions in some patients.
Procedure Details: During an MRI scan, patients lie on a table within a tunnel-shaped scanner equipped with a powerful magnet. It is crucial for patients to remain still and breathe calmly throughout the scan, and they may be instructed to hold their breath briefly during certain procedures. All metallic objects must be removed before entering the MRI room to avoid interference with the magnetic field, which can also damage magnetic storage devices such as credit cards and electronic media.
Types of MRI Systems:
Safety Considerations: MRI is contraindicated for patients with certain metallic implants such as pacemakers, cochlear implants, and cerebral aneurysm clips. It is also generally advised against for pregnant women in their first trimester, due to the potential risks posed by the strong magnetic field. For lactating mothers, there are no general restrictions; however, if a contrast agent is used, breastfeeding should be postponed until the agent is completely excreted from the body (typically 24 hours).
MRI scans are particularly effective for examining soft tissues and are extensively used to assess the spread of tumors following colonoscopy. The procedure may involve the administration of a contrast agent to enhance the distinction between diseased and healthy tissues. MRI scans typically last between 20 to 30 minutes and may involve various specialized techniques, such as:
Enhancements in MRI: Color coding in MRI, particularly in perfusion and functional MRI, significantly enhances the visualization and interpretation of images. This process, however, is time-consuming and heavily reliant on sophisticated computer software.

MRI is a crucial tool in medical diagnostics, with applications spanning across various systems:
Magnetic Field Strength: The efficacy of MRI is heavily dependent on the strength of the magnetic field, measured in Tesla (T), where one Tesla equals 10,000 Gauss. The uniformity and stability of the magnetic field are critical for producing high-quality images.
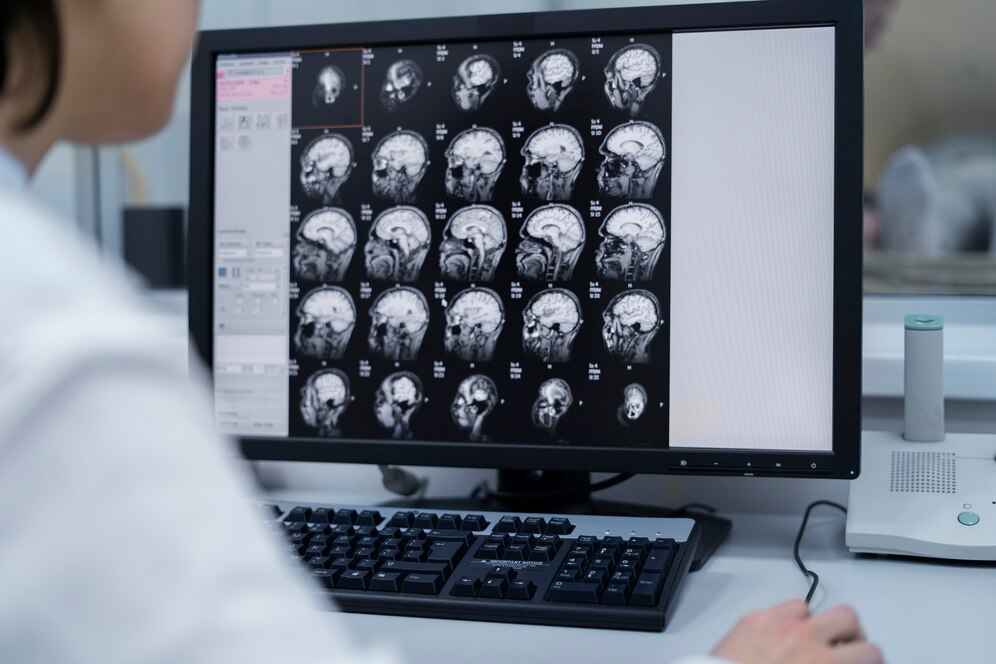
Cranial MRI
Cranial MRI is the most sensitive imaging technique for diagnosing chronic neurological conditions such as brain tumors, strokes, dementia, and multiple sclerosis. It excels in assessing the pituitary gland, cerebral vessels, eyes, and inner ear structures, and is instrumental in evaluating mental disorders due to its detailed examination of brain structures.

Magnetic Resonance Spectroscopy (MRS)
MRS is adept at detecting changes in cellular metabolites. This imaging technique performs biochemical analyses of pathological tissues and explores biochemical interactions within healthy tissues, providing a unique insight into cellular metabolism.
Diffusion Weighted MRI
Diffusion MRI captures images based on the molecular movement of water within tissue. Highly effective in diagnosing acute strokes, this technique surpasses CT and traditional MRI in detecting recent infarctions and aids in the differential diagnosis of intracranial cystic formations, and benign versus malignant spinal tumors, among other conditions.
Perfusion-Weighted MRI
Perfusion-Weighted MRI (PW MRI) reveals the functional state of brain tissue, highlighting hemodynamic alterations due to damage or space-occupying lesions. It is crucial for the non-invasive evaluation of strokes, intracranial tumors, dementia, cognitive disorders, and other physiological changes.
Functional MRI (fMRI)
Functional MRI is essential for surgical risk assessment and planning by mapping brain activity related to oxygen and blood supply. It is particularly valuable for preoperative mapping of brain regions associated with sensory, motor, and speech functions that are affected by space-occupying lesions.

MR Angiography
MR Angiography provides detailed imaging of blood vessels without the need for catheter insertion or radiation exposure. It is utilized for imaging intracranial vessels and those of the aorta, kidneys, lungs, arms, and legs.
Cardiovascular System MRI
This MRI modality assesses the structure and function of the heart and great arteries, including the dimensions and wall thickness of cardiac chambers, and the extent of damage due to myocardial infarction or progressive heart disease. It is increasingly used for coronary artery imaging, functional studies, and stress perfusion assessments.
Total Body MRI
Total Body MRI offers comprehensive imaging of major organs and blood vessels, including specialized studies like cholangiopancreaticography for detailed visualization of the gall bladder, bile ducts, and pancreatic duct without invasive procedures. It also serves as an alternative for imaging the reproductive and pelvic organs, including the urinary bladder.

Breast MRI
While not a replacement for mammography or ultrasound, Breast MRI complements these techniques in the early detection of breast tumors, evaluation of multiple tumor sites, and cancer screening in patients unsuitable for mammography due to factors like silicone implants or dense breast tissue.
Prostate MRI
Prostate MRI is used for diagnosing prostatitis, benign prostatic hyperplasia, and prostate cancer. It accurately assesses tumor size and spread, which are critical in treatment planning for biopsy-confirmed prostate cancer.
Musculoskeletal System MRI
This MRI modality provides detailed visualization of muscles, tendons, ligaments, joint structures, and soft tissues. It is invaluable for assessing sports-related injuries, joint disorders, arthritis, musculoskeletal tumors, and the spread of tumors to bones, as well as postoperative spinal conditions.

Preparation and Scan Phases of MRI
MRI scans typically require no special preparation. Patients may eat, drink, and take medications as usual unless advised otherwise. Prior to scanning, patients should complete a medical history form and remove any metal objects. If needed, they may empty their bladder. The scan duration ranges from 15 to 45 minutes, during which patients must remain still to ensure image clarity. Contrast agents may be used to enhance image quality and diagnostic accuracy.
Differences Between MRI and CT Scans
MRI (Magnetic Resonance Imaging) offers several advantages over CT (Computed Tomography) in various clinical conditions:

MRI holds distinct advantages over conventional radiological studies, including CT:
Inferiorities of MRI
Despite its advantages, MRI has limitations:
Higher Costs: The superior imaging quality of MRI comes at a higher price, driven by the cost of superconductor devices used in the scanners. However, advancements are also being made in developing more cost-effective technologies.

In clinical practice, MRI is extensively used for examining the central nervous system. Key applications include:

While mammography, complemented by ultrasound, remains the primary diagnostic tool for breast diseases, MRI is used as a secondary diagnostic tool when further detailed imaging is required. Mammography continues to be the gold standard for the early detection of breast cancer.
How Are Breast Cancer Diagnoses Made Using Mammography and Ultrasound? What Happens If Cancer Is Suspected? Mammography and ultrasound are fundamental tools for imaging the breasts. Radiologists, especially those proficient in digital imaging technologies, use these tools to distinguish between benign and malignant breast changes. Most lumps, often palpated by patients or physicians, are benign tumors or cysts, particularly common between the ages of 30 and 50. These benign conditions, such as fibroadenomas and cysts, can usually be differentiated from cancerous growths through ultrasound and mammography. If cancer is suspected, the radiologist will advise a biopsy and consult with the referring physician to determine the procedure for sample collection. Lumps deemed to have a very low risk of cancer are monitored with periodic ultrasound and/or mammography to confirm they do not grow or change, effectively ruling out cancer.
